 Over the past two years, the Women’s Health Institute
of the Allegheny Health Network (AHN) has followed a
phenomenal trajectory.
Over the past two years, the Women’s Health Institute
of the Allegheny Health Network (AHN) has followed a
phenomenal trajectory.
We have expanded our Centers of Excellence,
particularly in pelvic health and endometriosis, and
continue to build out our research portfolio.
In addition, AHN opened the second new labor and
delivery unit in the state of Pennsylvania in more than a
decade at AHN Wexford, for a total of five units. These
new facilities expand access to obstetric care in the
region at a time when dozens of labor and delivery units
have closed regionally over the past 20 years.
Throughout our network, we continue to provide patients
with expert routine and tertiary care in every subspecialty.
Our providers are focused on offering high-quality, stateof-
the-art care in a safe and compassionate environment,
from birth through midlife/menopause.
We hope the information on the following pages will
help you as you evaluate options for your patients. As a
well-established presence in the western Pennsylvania
community, we strongly believe the best possible
outcomes depend on our ability to build strong
relationships with you and your patients.
It is an honor to partner with you in the provision of
vital care to your patients, and we are here should our
services be of value to you.
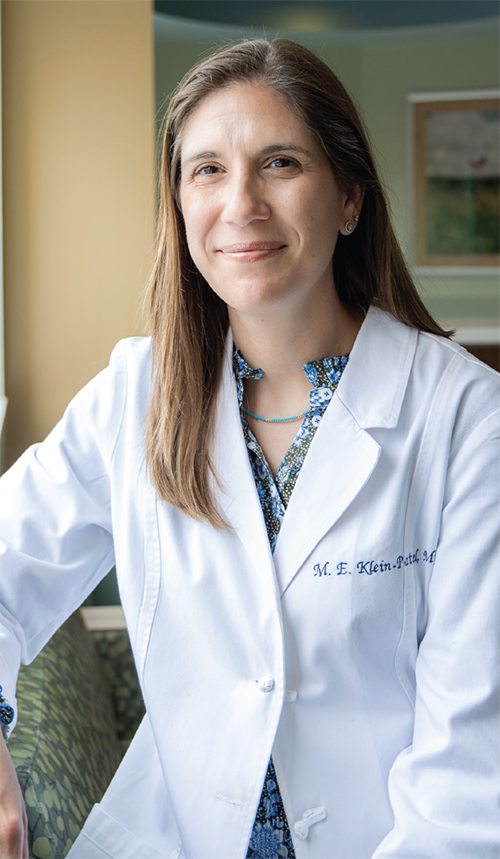
Marcia Klein-Patel, MD, PhD
Chair, AHN Women’s Health Institute
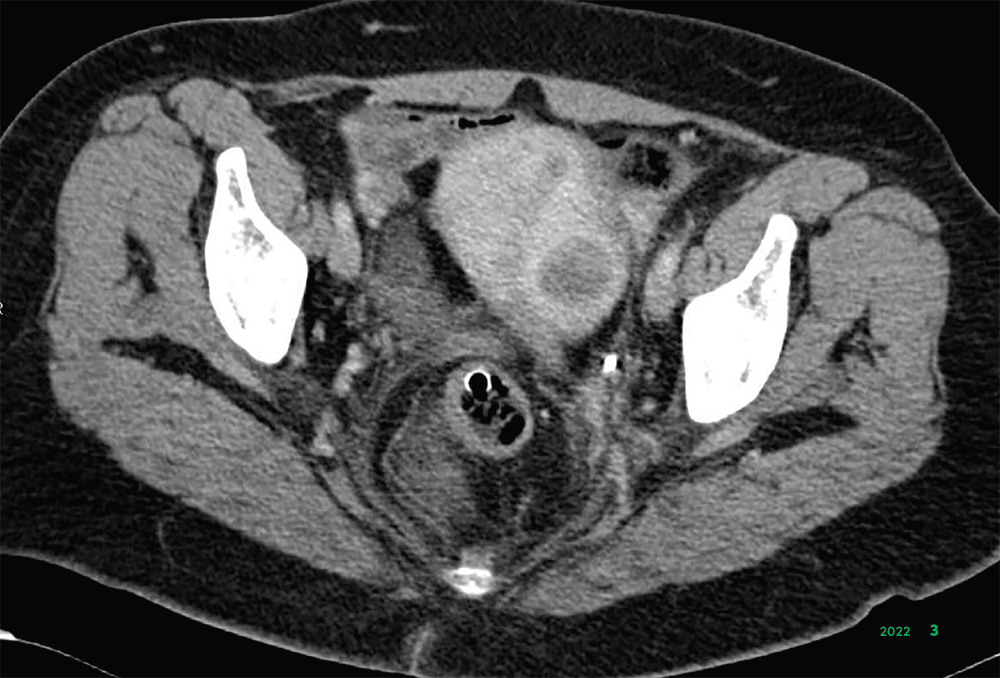 Allegheny Health Network (AHN) gynecologic surgeons
are using minimally invasive approaches in the removal
of uterine fibroids, which affect up to 70% of women.1
These often benign growths can have a significant
impact on women’s health, causing bleeding, urinary
incontinence, infertility and anemia.
Allegheny Health Network (AHN) gynecologic surgeons
are using minimally invasive approaches in the removal
of uterine fibroids, which affect up to 70% of women.1
These often benign growths can have a significant
impact on women’s health, causing bleeding, urinary
incontinence, infertility and anemia.
“Many patients underwent hysterectomies for
uterine fibroids, which had obvious implications
for reproductive health,” said Noah Rindos, MD, a
gynecologist with AHN. “Thankfully, we’ve advanced
beyond that. We’re now able to relieve these symptoms,
with minimal disruption to their lives.”
Indeed, at AHN, uterine fibroid removal is being
performed via minimally invasive laparoscopic
myomectomy, which involves four small incisions. The
procedure has fewer postoperative complications and
less postoperative pain than open surgery. Recovery
time is shorter; patients are usually discharged from the
hospital the day of the procedure.
“We’ve really made an effort to incorporate stateof-
the-art surgical approaches so that patients can recover and get back to their lives
quickly, with minimal
pain,” Dr. Rindos said.
Dr. Rindos and his colleagues have been working with
interventional radiologists Andrew Klobuka, MD, and
Benjamin Contrella, MD, to incorporate minimally
invasive embolization techniques into clinical practice
as part of developing AHN as a Center of Excellence for
uterine fibroids.
Uterine fibroid embolization uses fluoroscopy guidance
to deliver an agent that blocks the arteries that provide
blood to fibroids, causing them to shrink. Nearly 90% of
women who undergo the procedure experience significant
or complete resolution of their fibroid-related symptoms.2
“We’re excited to provide a collaborative approach
in the treatment of fibroids.” Dr. Rindos said. “While a
myomectomy is generally not considered lifesaving
surgery, I’ve had patients tell me after surgery that they
haven’t felt this well in years and have their lives back.”
1. J Womens Health [Larchmt]
2018;27[11]:1359-1367.
2. Insights Imaging 2022;13[1]:106.
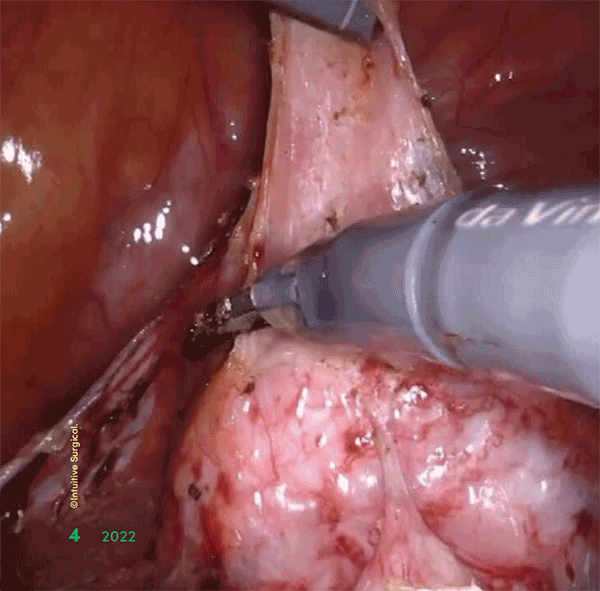 Gynecologic oncologists within the Allegheny Health
Network (AHN) Women’s Health Institute are using
state-of-the-art robotic technologies for minimally
invasive surgical treatment of benign and malignant
uterine conditions, as well as other diseases of the
reproductive tract.
Gynecologic oncologists within the Allegheny Health
Network (AHN) Women’s Health Institute are using
state-of-the-art robotic technologies for minimally
invasive surgical treatment of benign and malignant
uterine conditions, as well as other diseases of the
reproductive tract.
“Patients want to have their surgeries done robotically—
today, they expect that,” said Eirwen M. Miller, MD,
a gynecologic oncologist at West Penn Hospital, part
of AHN. “So many of our patients come to us having
done online research about surgical approaches
to hysterectomy. They know that many of these
procedures are being performed robotically. They
may not understand the specifics of the technology,
or the effect on surgical outcomes, but they know that
robotic surgery is the most contemporary approach to
gynecologic surgery.”
Demonstrating the system’s commitment to robotic
surgery, West Penn Hospital is equipped with four
surgical systems from Intuitive Surgical: one da Vinci
X® and three da Vinci Xis®. This investment means the
hospital has the most robotic surgical platforms of any
in the region, according to Dr. Miller.
First approved by the FDA in 2000, the newer
generations of the da Vinci Surgical System, like
those in use at West Penn, are designed to provide
surgeons with increased range of motion, dexterity and
visualization during procedures such as hysterectomy,
surgical correction of pelvic organ prolapse,
endometriosis resection and gynecologic cancer
surgery.
Additionally, gynecologic oncologists at the Women’s
Health Institute are using Firefly® near-infrared
fluorescence imaging for visualization of sentinel lymph
nodes. This technology is routinely used for endometrial
cancer staging surgery, reducing the incidence of
complete pelvic lymphadenectomy and associated
morbidities.
However, the term “robotic” is a bit of a misnomer
when describing procedures performed with the da
Vinci system, Dr. Miller noted. With systems such as da
Vinci, robots are not actually performing the surgery—
surgeons are. Surgical expertise is still needed to
interpret the images seen on the platform’s screen and
guide the robotic arms and instruments.
“Really, it provides the best of both worlds—the expertise
of skilled surgeons with the accuracy of 3D imaging and
robotic technology,” Dr. Miller explained.
With the four da Vinci surgical systems at surgeons’
disposal, about 60% of gynecologic oncology procedures
at West Penn are performed robotically, using minimally
invasive, laparoscopic techniques. According to
Dr. Miller, gynecologic surgeons perform approximately
two-thirds of the robotic surgery volume at the hospital.
“The technology has changed our practice,” she said.
“The fact that we have four da Vinci surgical systems
demonstrates our commitment to utilizing most
contemporary technologies, which are associated with
the best patient outcomes. From the patient perspective,
robotic surgery is associated with faster recovery, less
pain and surgical blood loss as well as lower infection
rates. This means we are providing our patients with the
best care possible.”
da Vinci X® is a registered trademark of Intuitive
Surgical and is
used with permission. da Vinci Xi® is a registered trademark of
Intuitive Surgical and is used with permission. Firefly® is a registered
trademark of Intuitive Surgical and is used with permission.
Midlife care has become a key component of the
services offered by the Women’s Health Institute within
Allegheny Health Network (AHN).
Too often, the specialty of women’s health focuses on
pregnancy and the health of women of childbearing
age, meaning patient care stops before menopause.
However, AHN’s Women’s Health Institute uniquely
includes specialists on staff who are focused specifically
on midlife, when a woman’s body undergoes changes
that can have significant effects on their health and
well-being, according to Marcia Klein-Patel, MD, PhD.
Although she is an obstetrician-gynecologist by
training, Dr. Klein-Patel, who is the chair of the AHN
Women’s Health Institute, stepped away from obstetrics
to focus on midlife care for women as they age. This
subspecialty includes everything from the management
of menopausal symptoms such as severe hot flashes,
vaginal dryness, and sexual and pelvic health to urinary
incontinence, bone loss and gynecologic cancers.
“When it comes to women’s health, we often talk about
reproduction, but we don’t talk enough about what
happens after women are no longer of reproductive
age,” Dr. Klein-Patel said. “Sometimes, these subjects
are difficult for women to talk about. However, we have
created an environment at all of our practice locations
where women can feel comfortable talking to our team
about any and all health-related issues as they age.”
To meet these needs, the midlife program at the
Women’s Health Institute features a multidisciplinary
team of specialists that includes gynecologists,
psychiatrists, psychologists, cardiologists,
gastroenterologists, oncologists, pelvic floor therapists
and sleep specialists, among others. The team ensures
patients in their care are maintaining a healthy diet,
exercising appropriately and receiving preventive
medicine services, including routine vaccinations as well
as cancer screenings.
“Our first priority is education—informing our patients
why these services are so important,” Dr. Klein-Patel
said. “After that, we want to help guide them through
steps they can take to make sure they are living their
best lives.”
Despite research highlighting the importance of midlife
care in women’s health1 and
studies indicating that
patients want these services,2
few health systems are
offering them.
“When a patient who is pregnant comes into an
obstetrician’s office, they often say they want to make
all of these health changes for their baby, which is
wonderful,” Dr. Klein-Patel noted. “However, when a
woman comes into my office, they realize they have
about half of their life left to live and they want to make
changes for themselves, and that’s so rewarding. It’s
great to walk that path with them.”
1. Menopause 2022;25(10):1155-1164.
2. J Womens Health [Larchmt] 2014;23[6]:513-518.

What’s better than having an excellent private-practice
fertility specialist when getting pregnant hasn’t been
easy? Having a team of specialists that may include a
reproductive endocrinologist, a high-risk obstetrician, a
pelvic floor physical therapist and a minimally invasive
surgeon, according to Lori Homa, MD, the medical
director of the Allegheny Health Network’s (AHN’s)
Center for Reproductive Medicine.
“Because of our connection to Allegheny Women’s
Health, we have a full scope of services for our fertility
patients at our fingertips,” she said. “We all work
together. It’s really nice to be able to offer that.”
The Center provides infertility care for all people
who wish to conceive, including same-sex couples,
transgender people, cisgender women with infertility
and those born with uterine abnormalities.
Dr. Homa uses her expertise to develop a personalized
journey for all patients that focuses on their unique
needs. She has extensive experience assisting couples
and individuals in conceiving in ways that work for
them, including utilizing eggs and sperm from donors,
transgender men and transgender women. The
Center prides itself on being an accepting space for all
individuals at every stage of their treatment.
Services include intrauterine insemination, in vitro
fertilization, pre-implantation genetic testing and
surgery for reproductive issues. The center’s success
rates are higher than the national average.
“We have a wide range and scope of treatments
available, and our embryologists are amazing,” Dr. Homa
said. “We offer exceptional care for all aspects of fertility
and for all people who want to expand their family.”
The Center also offers behavioral health counseling that
can begin with preconception counseling and provide
support throughout treatment.
Preconception counseling can enable physicians and
patients to prepare ahead of time for a variety of issues
that may arise either in treatment or during pregnancy,
and allows patients to be in the best physical and
emotional condition possible.
Plans are underway for the Center, which is currently
located at both Allegheny General Hospital and a
clinical practice in McCandless Township, to move to a
new facility in Robinson Township, with all services at
one location.
“For many patients, undergoing treatment can be an
emotional and stressful time,” Dr. Homa said. “Having
resources to support our patients both physically and
emotionally is important.”
 Some women wait years before addressing common
pelvic floor conditions such as pelvic organ prolapse,
pelvic pain and incontinence.
Some women wait years before addressing common
pelvic floor conditions such as pelvic organ prolapse,
pelvic pain and incontinence.
“There are women who have essentially chosen to be
confined to their homes because they’re afraid to have a
bowel or bladder accident in public,” said Lindsay Turner,
MD, a urogynecologist with Allegheny Health Network
(AHN) who specializes in female pelvic medicine and
reconstructive surgery. “Fortunately, we have advanced
treatment options available for women who have tried
first- and second-line therapies without success.”
Up to 20% of women in the United States will undergo
surgery for pelvic organ prolapse or stress incontinence
by the time they’re 80 years of age.1 Because these
conditions are more prevalent in postmenopausal women
whose pelvic floor disorders may be exacerbated by loss
of estrogen, it’s estimated that this number could rise to
50% by 2050 as the baby boomer generation ages.2
At AHN, Dr. Turner and her colleagues have helped many
women eliminate incontinence, ending their reliance on
pads or adult diapers and returning to their previously
active lives. They also work with women who develop
pelvic issues in the first 12 weeks after childbirth, a
period that the American College of Obstetricians and
Gynecologists has called “the fourth trimester.”
Fourth trimester issues can range from slow healing
obstetrical lacerations to painful intercourse, prolapse
and incontinence. Even women who have had a
cesarean delivery are recovering from a large-scale
surgery while caring for a newborn, and this can cause
significant physical and psychological stress.
“Urinary incontinence, prolapse and pelvic pain are
common in the postpartum period and can continue
for years afterwards; as pelvic floor specialists, we
can get involved earlier,” said Radhika Patnam, MD, a
urogynecologist specializing in female pelvic medicine
and pelvic pain. “The American College of Obstetricians
and Gynecologists has begun focusing on the fourth
trimester, and we hope to improve care during this
important time.”
Some women do not have easy access to pelvic floor
care. To address this issue, AHN urogynecologists
operate out of several satellite offices and hospitals,
including Hempfield, Bethel Park, Jefferson, Wexford,
Forbes and Allegheny Valley.
“We are seeing patients in their own communities so
that they have fewer barriers in accessing specialist
services,” Dr. Turner said. “It’s difficult for many patients
to navigate Pittsburgh, so we’re trying to overcome that
by going to them.”
For women seeking surgery, AHN urogynecologists offer
minimally invasive options such as vaginal, laparoscopic
and robotic surgery. For women who wish to avoid
surgery, our physicians may recommend office-based
procedures, pelvic floor physical therapy, behavioral
modifications or pharmacologic options.
“We are telling women these problems don’t have to be
a part of their daily lives,” Dr. Turner said. “We can make
a difference.”
1. Obstet Gynecol
2014;123[6]:1201-1206.
2. Obstet Gynecol 2019;134[5]:e126-e142.
 There has been an unprecedented increase in research
being conducted at the Allegheny Health Network (AHN)
Women’s Health Institute, with physicians leading multiple
clinical trials.
There has been an unprecedented increase in research
being conducted at the Allegheny Health Network (AHN)
Women’s Health Institute, with physicians leading multiple
clinical trials.
“Our physicians and specialists are leading a large
number of clinical studies in a number of therapeutic
areas,” said Thomas C. Krivak, MD, the director of
gynecologic oncology at AHN.
“Having access to clinical trials within our oncology
program is a cornerstone to offering our patients the best,
state-of-the-art care,” added Sarah Crafton, MD, the
director of the gynecologic oncology clinical trial program
and a gynecologic oncologist with AHN. “Over the past
five years, we have increased the number of open clinical
trials and the number of patients screened and enrolled.”

Although the field of reproductive infectious
disease has been around since the 1970s, it’s rare for
hospitals to have a specialist on staff.
At the Allegheny Health Network (AHN), Yasaswi
Kislovskiy, MD, brings that expertise to the Women’s
Health Institute, making sure patients receive the latest
evidence-based treatments while tackling the systemic
issues that place them at increased risk for reproductive
infections in the first place.
Dr. Kislovskiy's presence at the Women’s Health Institute
means patients have access to a highly trained specialist
for complex conditions at the intersection of gynecology,
obstetrics and infectious diseases. In addition, other
physicians can call on her specialized knowledge to
ensure even better care for their patients.
“Staying on top of the latest evidence-based
approaches is a critical part of my job and enables me
to provide highly specialized care for individual patients,”
Dr. Kislovskiy said.
Dr. Kislovskiy focuses on providing trauma-informed
treatment and the management of complex pelvic
inflammatory diseases. Gynecologic care for people
living with HIV and performing complex colposcopy
to prevent cervical cancer are also within her skill set.
An outpatient clinic treats patients who have chronic
vaginal infections, odor, itching, discharge and/or pain.
In addition to treating the symptoms of an infection,
Dr. Kislovskiy considers the larger systemic issues that lead
to infections and related health concerns. She also cares
for pregnant people in need of addiction-related support.
“We strive to combine technical expertise in treating
infections and peripartum challenges with a deep
knowledge of systemic issues and a focus on
preventative health solutions,” said Dr. Kislovskiy, who
is also co-director of AHN’s Perinatal Hope Program, a
collaboration between the Women’s Health Institute and
the Center for Inclusion Health. “Patients at the Women’s
Health Institute benefit from having access to a specialist
available at few other institutions in the United States.”
For patients who are gender diverse, nonbinary
and transgender, AHN’s Center for Inclusion Health
has expanded its gender-affirming medical and
surgical services, with a focus on providing access
in a convenient and compassionate way.
Specialists working within the Center include
plastic surgeons, endocrinologists, psychiatrists,
obstetricians and gynecologists, urologists,
orthopedists, and physical and occupational
therapists.
As needed, behavioral health providers and
social workers work side-by-side with specialists
to help patients cope with common and complex
mental health issues and social challenges. In
addition, providers work closely with patients’
health plans to make sure they cover researchbacked
services for gender affirmation.
AHN currently provides a wide range of primary
care services and certain gender-affirming
surgeries at multiple locations. Surgeons
have experience performing several types of
gender-affirming surgery, including breast
reduction/augmentation, chest reconstruction/
masculinization, orchiectomy, hysterectomy,
facial feminization surgery and trachea shave.
 Some pregnant people experience extreme
anxiety prior to cesarean delivery. This anxiety
can lead to elevated heart rates, hypertension,
difficulty breathing, panic and dissociation, all
of which can cause health complications for
both mother and child.
Some pregnant people experience extreme
anxiety prior to cesarean delivery. This anxiety
can lead to elevated heart rates, hypertension,
difficulty breathing, panic and dissociation, all
of which can cause health complications for
both mother and child.
In fact, up to 44% of pregnant women classify
their labor and delivery experience as
traumatic.1 In addition, a 2021
report from the
Centers for Disease Control and Prevention
found that nearly 10% of all maternal deaths
during infant delivery were linked to trauma
and mental health conditions—roughly the
same percentage as deaths attributed to
hypertensive diseases in pregnancy.2
“Treating these patients has introduced me
to the concept of trauma and post-traumatic
stress disorder and what it’s like for survivors
of trauma, especially childhood trauma, to go
through childbirth,” said Tracey Vogel, MD, an
obstetric anesthesiologist with Allegheny Health
Network (AHN).
The Women’s Health Institute offers pregnant
people experiencing childbirth-related trauma
comprehensive care that includes obstetric and
gynecologic services tailored to their specific
needs, as well as fully integrated behavioral
healthcare. The program addresses the need
for trust and control that these patients have,
and aims to improve their sense of self-worth
and self-efficacy.
These services are offered to patients within the
Obstetric Trauma Clinic at AHN, and the process
begins as early in pregnancy as possible. After
they are evaluated, patients work with the
clinical team to develop a birth plan that makes
them feel safe, Dr. Vogel added.
In general, the Obstetric Trauma Clinic follows
the “4 Rs of trauma-informed care” developed by
the Substance Abuse and Mental Health Services
Administration—realize the trauma, recognize its
impact on the patient, respond and resist retraumatization
in the birthing experience.
This approach to care is “a way of
understanding patients’ context, and then
tailoring what we do to minimize their concerns
or fears to get a better outcome,” Dr. Vogel said.
1. Acta Obstet Gynecol Scand
2018;97[6]:648-656.
2. Natl Vital Stat Rep 2020;69[2]:1-18.
For most expecting parents, pregnancy is typically a
time of joy. However, for those who have been told that
their baby has a life-limiting condition, it can be filled
with profound stress and grief. As a result, these families
require specialized care and need support services.
To meet these needs, Allegheny Health Network (AHN)
has established Olivia’s Angels, a perinatal palliative
care program designed for parents who have learned
their child may have a life-limiting or life-long condition,
or who have lost a child during the birthing process.
“We wanted to create a comprehensive, specialized
program that meets the unique needs of these parents,”
explained Marta Kolthoff, MD, a clinical geneticist
and an obstetrician-gynecologist in the maternal—
fetal medicine program within AHN’s Women’s Health
Institute. “Receiving such a diagnosis is devastating,
and to not have resources as you’re going through this
experience is challenging and traumatic.”
Olivia’s Angels was born out of Dr. Kolthoff’s role as a
geneticist working with pregnant people to assess their
risk for passing genetic disorders on to their children.
Unfortunately, she said, it’s the geneticist who ends up
informing parents that, as a result of genetic conditions
or fetal malformations, their baby’s life may be brief.
The program includes geneticists, maternal—fetal
medicine physicians, nurses and neonatal clinicians,as well as social workers, all of whom
have been
trained in perinatal death to ensure families receive
compassionate care. All services are customized
according to their individual needs and wishes, such as
religious requirements.
“We’ve learned that perinatal palliative care is much
more than just managing pregnancies,” Dr. Kolthoff said.
“We ensure these families are adequately supported.”
Approximately one in 300 newborns will have lifelimiting
diagnoses, according to the Centers for Disease
Control and Prevention. Although disorders such as
trisomy 18 or anencephaly are rare, they can collectively
affect many pregnancies.
For those who opt to deliver their babies, Olivia’s Angels
offers on-site support for both parents and families
as well as medical care for newborns. This support
also engages maternal—fetal medicine and newborn
medicine specialists. In addition, AHN’s Olivia’s Angels
Perinatal Palliative Care Program provides support for
families who can care for their newborns at home and
opt to do so.
“We’re expecting to have many more patients in Olivia’s
Angels, which is a difficult thing to say but important to
acknowledge,” Dr. Kolthoff said. “It really highlights the
need for pregnant people to have access to prenatal
diagnosis.”
 The Maternal—Fetal Medicine (MFM) and Newborn
Medicine programs within the Allegheny Health
Network (AHN) Women’s Health Institute work in tandem
to provide high-quality care for pregnant people and
their infants.
The Maternal—Fetal Medicine (MFM) and Newborn
Medicine programs within the Allegheny Health
Network (AHN) Women’s Health Institute work in tandem
to provide high-quality care for pregnant people and
their infants.
The MFM program has specialty programs for patients
with specific needs, support for medically complicated
pregnant people, palliative care, technical expertise
in obstetric ultrasound and reproductive genetics, and
patient navigation services to help guide them through
their healthcare journey. This work is connected to that
of the Newborn Medicine program, a department in the
Pediatric Institute with a tight-knit team that combines
cutting-edge technology with personal medicine to care
for all babies and their families after birth.
Over the past 30 years, the obstetrics and gynecology
practice at AHN has expanded from a single community
hospital with just over 2,000 deliveries annually to
a network with more than 8,000 deliveries a year,
according to Ron Thomas, MD, the division director of
the MFM program.
This expansion has allowed the AHN to invest in
specialty initiatives such as the Diabetes in Pregnancy
Program. Through this program, two full-time
certified nurse practitioners provide consultation
and management of pregestational and gestational
diabetes throughout the network, under the supervision
of MFM specialists. In addition, the Alexis Joy D’Achille
Center for Perinatal Mental Health, through the Institute
of Behavioral Health, is one of just two programs in
the nation that offers care for mothers in cases of
postpartum depression. The MFM team is also involved
with the Perinatal Hope Program, which coordinates
antepartum and postpartum care for patients with
substance use disorders.
“The MFM staff are experts at medically complicated
pregnancies and serve as a resource for other
physicians in the network,” Dr. Thomas said. “For
example, we have developed a detailed handbook for
all practices in the network, explaining the conditions
most likely to cause issues during labor.”
Technical expertise is also a key component of the
MFM program. At AHN, all obstetric ultrasounds are
performed by ultrasound technicians specially trained
in obstetrics and gynecology and overseen by MFM
physicians. This approach enables providers to find
abnormalities earlier in the pregnancy, giving the
patient and their care team time to plan for an optimal
delivery, according to Dr. Thomas.
In addition, the MFM program offers genetic testing
and includes a board-certified medical geneticist,
Marta Kolthoff, MD, who counsels patients so they can
understand the details of both the testing process and
the test results.
The program also provides hands-on guidance for
patients navigating the healthcare system. A nurse
navigator within the MFM department coordinates
consults, appointments, and transfers of care between
centers. Patients who need to deliver at a tertiary care
site have access to multi-specialty coordination of care
to plan their delivery.
For babies born prematurely, those with congenital
issues, or babies who have an infection, the Newborn
Medicine program has the tools to provide lifesaving,
hands-on care. The physical footprint of the Newborn
Medicine program includes two level 3 neonatal
intensive care units (NICUs), the highest level of
certification a community hospital can achieve, located
at two large centers: West Penn Hospital and Saint
Vincent Hospital. The network includes several level 2
NICUs to care for babies who require less intensive care
and attention, as well as regular newborn nurseries
(level 1 NICUs) for healthy infants at every hospital in
the network.
“The goal of the Newborn Medicine program is to
provide care to all the newborns born in the AHN
system, from the healthiest to the sickest,” said William
McCarran, MD, the director of the Newborn Medicine
program. “The program provides very complex, highlevel,
family-centered care. The team provides cuttingedge
care for the baby while also getting to know and
caring for the baby’s family.”
The Obstetrics and Gynecology Residency Program
at the Allegheny Health Network (AHN) Women’s
Health Institute strives to train residents to become
compassionate, ethical physicians and surgeons
committed to life-long learning and excellent patient
care.
Led by program director and urogynecologist Erin
Seifert Lavelle, MD, the accredited four-year program
welcomes six residents annually, and is primarily based
out of AHN’s West Penn Hospital in central Pittsburgh.
“Historically, we identified as a community program
and most of our graduates went on to practice general
OB-GYN. We really value OB-GYN specialty care and
provide training that prepares young physicians to
be exceptional OB-GYN physicians,” Dr. Lavelle said.
“However, we also have a long history of encouraging
scholarly activity, and are tremendously fortunate
to have an endowment from the James and Marilyn
Gilmore family dedicated to supporting resident
education and research.”
Residents participate in research and quality
improvement projects that impact the institute and
AHN, as well as advocacy and legislative work. Many
present their research nationally and publish in medical
journals.
“In recent years, we have adopted a blended
community-academic model, anchored by our core
faculty and bolstered by our academic partnerships,”
which include teaching responsibilities for students from
Drexel University College of Medicine, and a research
partnership with Johns Hopkins University,” Dr. Lavelle
said. “Our program definitely provides residents the platform to go on to fellowship
training if they choose;”
and the last three candidates who have applied for
fellowships have matched with leading subspecialty
programs, including gynecologic oncology at University
of Buffalo and urogynecology at Northwestern
University and Johns Hopkins University.
The heart of the program remains robust clinical
training. By design, according to Dr. Lavelle, residents
are integrated into patient care from their first day
within the program, with support from faculty and
advanced practice providers.
This latter group includes treatment of pregnant people
with substance use disorder as well as transgender and
midlife or perimenopausal care, she added. As a Ryan
Foundation Grant program, there is also an emphasis
on complex family planning care.
Part of their training that goes beyond patient care
includes work in patient advocacy and hospital
leadership. AHN Women’s Health Institute residents
oversee students from Drexel University College of
Medicine and graduate as skilled clinical instructors
as well as physicians. Regardless of the career path
residents leaving the program ultimately choose,
the program emphasizes hands-on, comprehensive
training in the field.
“Because we’re incredibly busy here and offer every
subspecialty, our residents are deeply involved across
the entire spectrum of obstetrics and gynecology,”
Dr. Lavelle said. “That hands-on experience is what
draws our residents here, and it gives them the
technical experience to succeed wherever their career
path takes them.”

 For the past five years, the Allegheny
Health Network’s (AHN) Women’s
Health Institute has used data to
change the way women experience
obstetric and gynecological care.
For the past five years, the Allegheny
Health Network’s (AHN) Women’s
Health Institute has used data to
change the way women experience
obstetric and gynecological care.
“We work in the only field that sees
patients come into the hospital looking
forward to something and leaving
with something better—a baby,” said
Bernard Peticca, MD, the patient
experience officer for the Women’s
Health Institute. “If we can’t provide a
good patient experience, shame on us.”
As part of an ongoing process of
evaluation and improvement, every
patient who leaves the Women’s
Health Institute receives a 40- to
70-question survey. Dr. Peticca’s
team analyzes the data from patient
responses to determine where doctors
and staff can improve within 11 major
focus areas, including facilities, patient
communication, discharge planning
and follow-up care.
For example, AHN has made a
concerted effort to invest more time in
patient education to provide nursing
mothers “with a better understanding
of how to take care of their own
health,” Dr. Peticca said. In nursing
mothers with hypertensive disorders of
pregnancy, the right medication can
prevent both maternal and newborn
delivery complications.
In addition, Women’s Health Institute
obstetricians are emphasizing
what they call the fourth trimester,
increasing communication with
mothers during the first six to eight
weeks after delivery.
 “We want our patients to have the best
possible experience,” Dr. Peticca said.
“We’re also carefully looking at our
patient’s feedback to assure that all
the improvements and advances that
we’ve achieved in patient experience
are reaching all groups with total
inclusion and no barriers.”
“We want our patients to have the best
possible experience,” Dr. Peticca said.
“We’re also carefully looking at our
patient’s feedback to assure that all
the improvements and advances that
we’ve achieved in patient experience
are reaching all groups with total
inclusion and no barriers.”
Copyright © 2023 All rights reserved.
McMahon Group unless otherwise noted.
Reproduction in whole or in part without permission is prohibited.
McMahon Custom Healthcare Communications is part of McMahon Group.