 Dear Friends and Colleagues:
Dear Friends and Colleagues:
These are exciting times for the Allegheny Health
Network Neuroscience Institute.
Our neurologists are leading efforts to expand the use
of the latest innovations in the diagnosis and treatment
of neurologic disorders ranging from amyotrophic
lateral sclerosis and epilepsy to movement disorders
and multiple sclerosis (MS).
Similarly, our neurosurgeons are incorporating
cutting-edge technologies into spine procedures and
pioneering new approaches in the field of neurooncology.
We have long maintained busy programs in movement
disorders, headache and MS, and we’re now seeing
phenomenal growth in spine surgery, interventional
stroke, brain tumor and epilepsy, particularly as we
recruit some of the best-trained specialists in these
areas into our center.
We continue to provide our patients with the best care in
the region, and we hope the information on the following
pages will help you as you evaluate options for your
patients. With our long history in western Pennsylvania,
we strongly believe the best possible outcomes depend
on our ability to build strong relationships with you and
your patients.
It is an honor to partner with you in the delivery of stateof-
the-art treatment to your patients, and we are here
should our care and services be of value to you.
Donald Whiting, MD
Chief Medical Officer, Allegheny Health Network (AHN)
President, Allegheny Clinic
Chair, AHN Neuroscience Institute
 Patients at Allegheny Health Network (AHN) who suffer
ischemic stroke, hemorrhagic stroke and ruptured
brain aneurysms have access to new technologies and
procedures that promise faster care and yield better
outcomes.
Patients at Allegheny Health Network (AHN) who suffer
ischemic stroke, hemorrhagic stroke and ruptured
brain aneurysms have access to new technologies and
procedures that promise faster care and yield better
outcomes.
In ischemic stroke, neurologists within the network are
using several novel medications that are capable of
“opening up blood vessels faster and more efficaciously,”
according to Russell Cerejo, MD, the medical director for
stroke and the co-director of endovascular services at the
AHN Cerebrovascular Center.
In addition to these novel therapies, new approaches to
magnetic resonance imaging (MRI), such as hyperacute
MRI, help better identify ischemic stroke patients who
can benefit from treatments by accurately determining
the duration of their stroke (including time of onset).
“There have been studies showing that if you use MRIs
to characterize the stroke, you can guesstimate when
the stroke happened and whether it happened within
four hours,” Dr. Cerejo said. “Here at AHN, we’ve been
using MRIs for those specific patients who typically
would not be candidates for IV thrombolysis.”
In addition to pharmacologic interventions, there are
new surgical implants that are designed to open up
occluded blood vessels more quickly, added Richard
Williamson, MD, the director of the Cerebrovascular
Center at AHN. As an example, neurosurgeons at the
center are incorporating novel catheter technology into
clinical practice. These newer catheter designs can be
implanted into increasingly smaller blood vessels safely,
according to Dr. Williamson.
“We now have catheters that we can safely put in
smaller and smaller vessels in order to perform stroke
thrombectomies, where we go through the vessel and
actually open up where it has been blocked by a clot
or plaque,” he said. Having access to smaller catheters
allows surgeons to safely treat more patients who are
affected by stroke, he added.
Similar advancements have also improved outcomes
in patients with hemorrhagic stroke and ruptured
aneurysms, allowing neurosurgeons to use minimally
invasive options. For example, AHN neurosurgeons
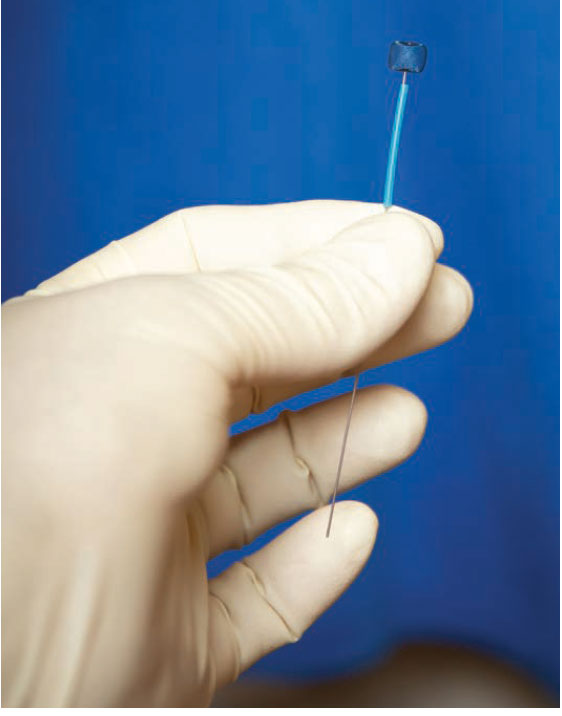
are now using a new technology called the Woven
EndoBridge (WEB™; Sequent Medical; pictured) for
these notoriously difficult-to-treat aneurysms.
As the name suggests, the WEB™ is an ellipsoid
braided-wire embolization device designed to provide
flow disruption along the neck of the aneurysm to
induce aneurysmal thrombosis.
“Wide-neck aneurysms are probably some of the most
challenging aneurysms that we see,” Dr. Williamson
said. “The WEB™ device has revolutionized the
way that we can treat wide-neck aneurysms. These
were typically aneurysms for which we had to do a
craniotomy.”
AHN neurosurgeons are also using a noninvasive
approach to treat subdural hematomas. The new
approach allows surgeons to “embolize or essentially
glue off vessels that are going up to that membrane,”
meaning patients no longer have to undergo
craniotomy for evacuation, according to Dr. Williamson.
The Cerebrovascular Center is participating in a
clinical trial to evaluate the safety and efficacy of this
artery embolization procedure compared with a more
traditional approach.
“With just a needlestick in the artery in the wrist, we can
go in and block off these vessels and the hematoma will
go away over the course of a few weeks,” he said. “This
has been a game changer for the neurosurgical field
because it’s been such a challenging entity for us to
treat. We’ve seen really great results, and patients often
don’t need surgery. Even if they do need surgery, they’re
much less likely to have problems long term.”
Woven EndoBridge (WEb)™ is a trademark of Sequent Medical and is used
with
permission.
 Across neuroscience, specialists are working to identify
ways to make surgery less invasive and to support faster
and better patient recovery.
Across neuroscience, specialists are working to identify
ways to make surgery less invasive and to support faster
and better patient recovery.
“The shorter and less invasive a surgery is, the faster the
patient recovers; they do better,” said Alexander Yu, MD,
vice chair of neurosurgery with the Allegheny Health
Network (AHN).
Neurosurgeons at AHN have long led the way in sameday
surgical procedures for the treatment of spine
disorders. Emerging technologies that allow surgeons to
avoid open procedures can minimize surgical wounds
and affect how quickly patients recover postoperatively,
according to Dr. Yu.
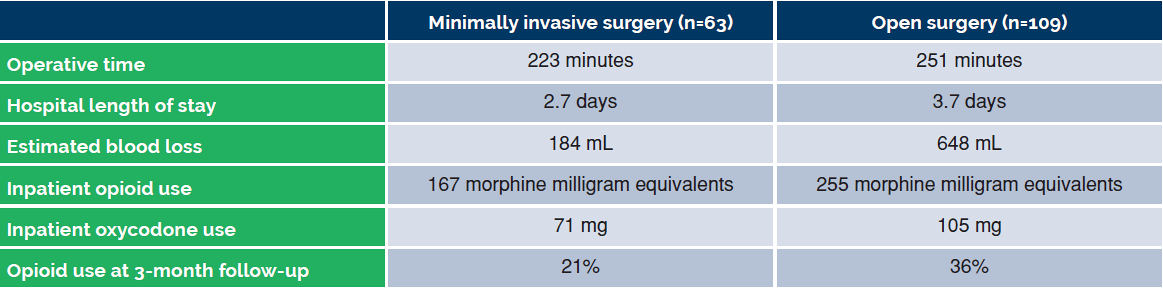
Indeed, minimally invasive approaches in spine surgery
have been associated with a reduced need for opioids,
decreased blood loss, shorter hospital length of stay
and fewer complications (Table).1.2 Robotic tools, such
as the Mazor X™ (Medtronic), enable more efficient
surgeries and faster recovery times by assisting
preoperative planning and intraoperative guidance, Dr.
Yu said.
Pain management is also greatly improved with sameday
procedures.
“We have an extended recovery anesthesia protocol,”
Dr. Yu noted. “When a patient comes in for surgery, the
protocol optimizes the recovery to focus on pain control
and optimize function. We’re developing more of these
protocols to increase the number of patients that can
go home the same day. About 20% of our neurosurgery
patients go home the same day—a figure that’s
probably doubled in the past five to 10 years.”
Generally, patients recover better at home, Dr. Yu said.
However, allowing patients to recover at home means
establishing protocols that help them to do so safely.
“Healing is better at home, and that’s where medicine
is moving,” he said. “Obviously, the No. 1 goal is always
going to be patient safety. As technology improves,
we can send more patients home the same day, while
keeping them safe.”
1. Global Spine J 2019;9[6]:624-629.
2. Spine [Phila Pa 1976] 2021;46[1]:62-68.
“Healing is better at home, and that’s
where medicine is moving. Obviously, the
No. 1 goal is always going to be patients
safety. As technology improves, we can
send more patients home the same day,
while keeping them safe.”
—Alexander Yu, MD,
AHN vice chair of neurosurgery
Table. Postoperative Complications: Minimally Invasive Surgery Versus Open Transforaminal Lumbar Interbody Fusion1

Neurosurgeons at Allegheny Health Network (AHN) are using state-of-the-art technologies that enable them to practice at the leading edge of neuroscience. Examples are described below.
Traditional surgery for tumors of the boney spine is
significantly invasive and requires removing tumor-filled
bone and, often, placing instrumentation into the spine to
stabilize it, said Nestor Tomycz, MD, a neurosurgeon with
the AHN. Medtronic OsteoCool™ uses radiofrequency
energy, delivered via two small probes placed into the
bone, to heat and ablate cancerous and benign tumor
tissue. Circulating water keeps the temperature stable
at the active tip to prevent thermal damage outside
the zone of ablation. The minimally invasive approach
reduces operative time, allowing patients to recover
faster, according to Dr. Tomycz. It can also be combined
with traditional vertebroplasty or kyphoplasty.
“The patient can go home the same day because we
can avoid large incisions and reduce blood loss,” he said.
“As a center, we’ve been dedicated to less invasive
spinal surgery and faster patient recoveries—it’s part of
our overall dogma in spine health.”
Indeed, a post-marketing study showed sustained
decreases in pain and increases in quality of life among
patients with metastatic bone disease who were treated
with OsteoCool™ tumor ablation.1
When a patient presents with an ischemic stroke,
a perfusion scan indicates the extent of damaged
versus salvageable tissue, information that helps
guide treatment decisions. RapidAI® is an automated,
artificial intelligence-driven software platform that
analyzes computed tomography and magnetic
resonance scans, providing critical information to
stroke interventionists and neurosurgeons within
minutes. Physicians at AHN are using the technology
to make treatment decisions when time is of the
essence, according to Russell Cerejo, MD, medical
director for stroke and the co-director of endovascular
services at the health system’s Cerebrovascular
Center. This effectively allows more patients to be
candidates for acute stroke intervention, which can
prevent permanent damage. In two studies presented
by Dr. Cerejo and his colleagues during the 2022
International Stroke Conference, RapidAI® showed
high sensitivity and specificity for detecting large
vessel blockages or severe narrowing as well as
hemorrhagic strokes very quickly, allowing for faster
triage, reducing time to treatment and improving
patient outcomes.2,3
“When a patient is having a stroke, every minute
counts because brain cells are dying,” Dr. Cerejo said.
“RapidAI® provides us with automated maps that can
tell us what part of the brain is affected.”

Synaptive’s Modus V™ robotic exoscope facilitates
surgical visualization and magnification in
neurosurgical procedures. The exoscope supports better
ergonomics allowing surgeons to comfortably access
and view difficult regions of the brain and spine and
aids in teaching and instruction, according to Richard
Williamson, MD, the director of the Cerebrovascular
Center at AHN.
Modus V™ is a 3D robotic exoscope tool that surgeons
can position anywhere in the surgical field, allowing
them to view difficult angles with the traditional
microscope, he said. The technology enhances surgical
ergonomics, meaning procedures can be performed
accurately, in less time, and with less physical strain on
the surgeon.
“It has broad applications”, said Dr. Williamson. “Anytime
we are using an operating microscope or are in a case
that requires magnification and illumination to operate
precisely—whether that’s in spine surgery, intracranial
cerebrovascular surgery or brain tumor surgery—the
exoscope is incredibly useful.”
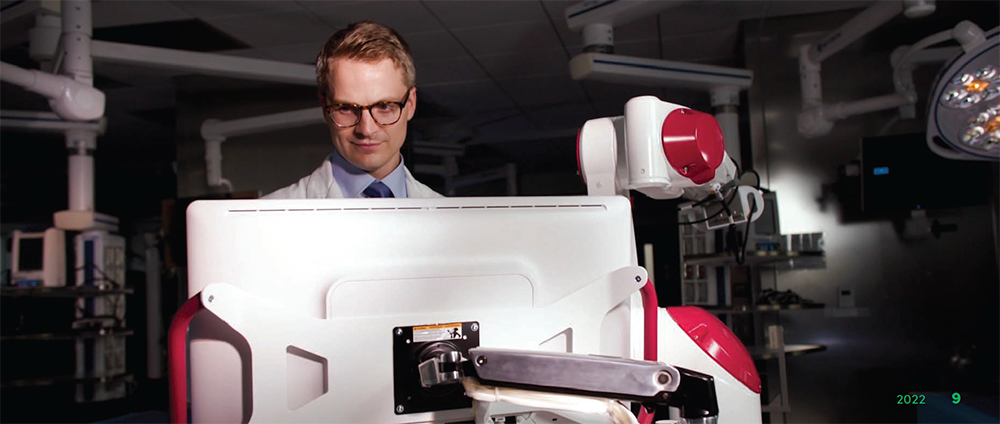
During spinal fusion surgery, screws are placed into the
bone to prevent motion between vertebrae to facilitate
fusion. Mazor X™ (Medtronic) helps surgeons ensure
accurate and efficient screw placement during this spinal
surgery. A major benefit of the Mazor X™ system is that
it allows surgeons to plan a trajectory before surgery
begins, according to Alexander Yu, MD, a neurosurgeon
with the AHN. A meta-analysis found that robotic
guidance with the Mazor X™ yields superior accuracy
and less blood loss compared with computer-assisted
navigation for pedicle screw placement.4
“We’re early adopters in terms of utilizing
technology,”
Dr. Yu said. “With platforms such as Mazor X™, there are
fewer surprises for the surgeon and better outcomes for
the patient.”

1. J Vasc Interv Radiol 2020;31[11]:1745-1752.
2. Abstract WMP68: International Stroke Conference 2022.
3. Abstract WP129: International Stroke Conference 2022.
4. World Neurosurg 2021;146:e139-e150.
Osteocool™ is a trademark of Medtronic and is used with permission. RapidAI® is used with permission of RapidAI. Modus V™ is a trademark of Synaptive Medical and is used with permission. Mazor X™ is a trademark of Medtronic and is used with permission.
Advancements in the surgical management of epilepsy
are allowing specialists to offer safe, effective, minimally
invasive treatment options for patients with difficult-totreat
drug-resistant disease.
According to the CDC, an estimated 3.4 million people
in the United States have epilepsy, and up to 40% of
them have drug-resistant disease.1
“Most epilepsy patients will respond to treatment and
will be cured, or at least live very functional lives,”
said Alexander C. Whiting, MD, a neurosurgeon and
the director of epilepsy surgery for Allegheny Health
Network (AHN) Neuroscience Institute. “However,
a large group of patients with medically refractory
epilepsy have a very significant disease that affects
their life span, makes it difficult to be employed and
greatly complicates their lives. During the past five to 10
years, we have developed some incredible options for
treating these people, all of which we offer at AHN.”
The primary diagnostic intervention is robotic
stereoelectroencephalography (SEEG), a highly
technical procedure that utilizes a robot to place
electrodes directly into a patient’s brain. The technique,
Dr. Whiting noted, is safe, has a very low complication
rate and allows the care team to identify the region of
the brain that is triggering a patient’s epilepsy.
“If we can localize where a patient’s epilepsy is coming
from, we can treat it,” Dr. Whiting said.
Key to these treatment plans are minimally invasive techniques such as responsive
neurostimulation (RNS)
and laser interstitial thermal therapy (LiTT).
RNS Therapy, which was approved by the FDA in 2013,
is similar in approach to a pacemaker used to control
irregular heart rhythms. A brain–computer interface
is created, consisting of a small computer and battery
that are imbedded under a patient’s skin. Electrodes are
then placed in the patient’s brain, targeting the region
causing seizures.
When the technology identifies the onset of a seizure, it
modulates the seizure, stopping it before it begins.
“RNS can significantly reduce the number of seizures a
patient has, sometimes completely stopping them,” Dr.
Whiting said.
If patients have epilepsy coming from a deep part of
the brain, surrounded by important functional areas,
LiTT allows surgeons to remove a seizure focus area
with pinpoint accuracy. In LiTT, a laser is placed deep
into the brain via a single, small incision, and is targeted
toward the region of the brain causing the patient’s
seizures, according to Dr. Whiting.
“We are getting much better at using existing technologies,
such as RNS, LiTT and SEEG, to tailor treatment, localizing
epilepsy for each patient and minimizing the amount of
surgery they need,” Dr. Whiting said. “At AHN, we have built
out the newest and most innovative technologies, which
have given us a whole new toolbox to treat epilepsy.”
1. Medicine [Baltimore] 2019;98[30]:e16402.
 The Allegheny Health Network (AHN) Neuroscience
Institute continues to evolve as a major research center.
The Allegheny Health Network (AHN) Neuroscience
Institute continues to evolve as a major research center.
“Over the past five years, our involvement in clinical
trials has grown by 20% to 30% annually, and we expect
it to continue to grow,” said Donald Whiting, MD, the
chief medical officer of AHN, president of the Allegheny
Clinic and chair of the AHN Neuroscience Institute.
Neuroscience Institute researchers are at the
forefront of efforts to expand the use of deep brain
stimulation (DBS).
The Institute is leading a small study in which
DBS will be used on three patients with opioid
use disorder who have relapsed after successful
rehabilitation. The Institute, is also leading a
small study of DBS in patients with obesity and
participating in a multicenter study of this approach
in the treatment of Alzheimer’s disease (ADVANCE II).
DBS uses electrodes implanted adjacent to specific
deep brain structures. The electrodes are connected
to a pacemaker-like device implanted on the chest
wall that delivers low levels of electrical stimulation
via a subcutaneous wire.
For patients with opioid use disorder and obesity,
researchers will be using the approach to target
the nucleus accumbens, a brain region believed to
be involved in the “reward” process. By delivering
electrical pulses there, researchers believe they can
help block cravings for opioids and unhealthy foods.
In patients with Alzheimer’s, DBS will target the
fornix, a brain region involved in memory, to reverse
some declines in cognitive function.
“We do a high volume of DBS in Parkinson’s disease,
and our experience with the approach has brought
us to this point, where we can be taking the lead on
studies of its use in new areas,” said Nestor Tomycz,
MD, the director of stereotactic and functional
neurosurgery. “That says our center is at the forefront
of using this technology.”

Neurosurgeons at the Allegheny Health Network (AHN)
Neuroscience Institute are incorporating cutting-edge
surgical techniques designed to improve outcomes in
patients with deep-seated and/or recurrent brain tumors.
Surgeons are using laser interstitial thermal therapy
(LITT), a minimally invasive technique developed to treat
epilepsy and other seizure disorders, in patients with
glioblastoma or metastatic tumors to effectively perform
“resection without incision” for faster recovery times,
according to Matthew Shepard, MD, the director of
brain tumor research at the AHN Neuroscience Institute
and a neurosurgeon in the Allegheny Health Network.
“LITT is an emerging option for patients whose
tumors may be more challenging for open surgical
resection,” Dr. Shepard said. “It also has the added
benefit of faster recovery time, which enables them
to start adjuvant therapy—whether it’s chemotherapy,
radiotherapy or immunotherapy—earlier, which further
improves outcomes.”
For patients who require open tumor resection, Dr.
Shepard and his colleagues are increasingly performing
awake craniotomies, during which patients remain
awake for accurate mapping of the tumor.
In addition, they are using state-of-the-art imaging
technologies, such as intraoperative ultrasound and
tumor fluorescence, to “maximize the degree of
surgical resection in these patients,” Dr. Shepard said.
Essentially, these technologies enable surgeons to
remove more of the tumor tissue without affecting the
surrounding nerves and brain tissue, he said.
“Intraoperative ultrasound allows us to look at tumors in
real time and to accurately assess degrees of resection,
while tumor fluorescence enables better visualization of
the tumors intraoperatively, basically by making them
glow in the dark,” Dr. Shepard explained. “With these
technologies, we are really trying to push the boundary
on degree of surgical resection because, in general, we
know the more tumor you can remove, the better patients
will do in terms of progression-free and overall survival.”
Conversely, these technologies also ensure surgeons
remove the “appropriate amount of tumor, without
causing a neurologic impairment, such as worsening
speech, which would obviate the benefits of resection,”
he added.
Another technique seeing increased use at the AHN
Neuroscience Institute is neuroendoscopy. According
to Jody Leonardo, MD, the director of the AHN Adult
Hydrocephalus Center and associate director of
endoscopic neurosurgery, the approach allows
surgeons to visualize and remove blood clots and brain
tumors through a small incision that is “about the size
of a nickel.”
“LITT is an emerging option for patients whose tumors may be more challenging for open surgical resection.”
—Matthew Shepard, MD, director, AHN brain tumor research
Dr. Leonardo and her team found particular success
with this approach in adults with hydrocephalus, which
is caused by an accumulation of cerebrospinal fluid in
the brain.
“With neuroendoscopy, we’re able to individualize
patient care and provide treatment in a minimally
invasive way, without craniotomy or other open surgery,”
Dr. Leonardo said.
As important as these technologies and novel approaches
are to surgical outcomes at the AHN Neuroscience
Institute, the most important tool the center has is its team
of skilled surgeons, according to Dr. Shepard.
“It’s not just having the right technology, but it’s having
the right technology in the right hands,” he added.
“We have the best surgeons in the tri-state region and
we know how to tailor our approaches to get the best
outcome for the patient in front of us.”
 The team of award-winning experts at the Allegheny
Multiple Sclerosis Treatment Center at Allegheny
General Hospital are involved in clinical trials and
taking “deep dives” into outcomes data to incorporate
the latest treatment options for patients with multiple
sclerosis (MS).
The team of award-winning experts at the Allegheny
Multiple Sclerosis Treatment Center at Allegheny
General Hospital are involved in clinical trials and
taking “deep dives” into outcomes data to incorporate
the latest treatment options for patients with multiple
sclerosis (MS).
“We aim to bring to our patients the latest
recommendations and treatments for patients with
immune disorders,” said Thomas Scott, MD, the director
of the Allegheny Multiple Sclerosis Treatment Center,
part of the Allegheny Health Network (AHN). “We’ve
been studying pharmacological approaches using
preapproval medications for three decades at AHN,
and have been collecting data for about 25 years
concerning disease behavior.”
“We’ve been studying pharmacological approaches using preapproval medications for three decades at AHN, and have been collecting data for about 25 years concerning disease behavior.”
—Thomas Scott, MD, director, Allegheny Multiple Sclerosis Treatment Center
For example, a new class of immune-altering drugs
that includes Bruton tyrosine kinase inhibitors are being
tested as a potential “missing link” in the management
of MS, due to the fact that they target both innate and
adaptive arms of the immune system.1
While dozens of medications are approved to treat
various aspects of MS, investigators are at work
studying which drug regimens might be best for
individual patients. The TREAT-MS trial,2 which is being
conducted at the Johns Hopkins University and counts Dr. Scott as an investigator, is addressing
an existing
lack of evidence-based guidelines to help clinicians and
patients determine which treatment strategy is best for
an individual with MS.
TREAT-MS Trial is a randomized, controlled trial that
plans to recruit 900 patients from more than 4o sites
across the United States, including AHN. In order to be
eligible, participants must have relapsing-remitting
MS and be between the ages of 18 and 60 years.
Participants who have been exposed to one or more
MS disease-modifying therapies, or have had prior
treatment with rituximab, ocrelizumab, ofatumumab,
alemtuzumab and/or an experimental aggressive
therapy, for more than six months are not eligible.
The goal of the trial is to determine whether some
patients would benefit from early, possibly more risky
aggressive therapy or if starting with a less aggressive
(and, often, less risky) therapy, followed by a switch
if breakthrough disease activity occurs, is optimal. In
addition, the study will strive to identify short-term
biomarker(s) strongly predictive of long-term disability
from MS.
In addition to participation in clinical drug trials, the
team is involved with research on disease behavior
using data on patient outcomes, looking specifically atrisk
factors for disease progression—as well as which of
these risk factors may be modifiable.
“My generation of doctors has seen a tremendous
improvement in the prognosis of MS patients and have
changed the natural history of the disease to greatly
reduce outcomes for long-term disability,” Dr. Scott said.
“The teaching mission of AHN allows us to teach these
up-and-coming doctors the latest regarding how to
take care of MS patients.”
1. CNS Drugs 2022;36[10]:1019-1030.
2. The TREAT-MS trial:https://treat-mstrial.org/.
 In recent years, advances in both pharmacology and
patient monitoring have enabled breakthroughs in
the management of a notoriously difficult condition—
chronic migraine.
In recent years, advances in both pharmacology and
patient monitoring have enabled breakthroughs in
the management of a notoriously difficult condition—
chronic migraine.
“Typically, with migraines we’ve had to treat patients
both with preventive medications and other drugs
aimed at targeting headache attacks,” said Andrea
S. Synowiec, DO, the system vice chair for Allegheny
Health Network’s (AHN’s) Neuroscience Institute.
“Historically, that has meant that patients like the attack
medicines because they feel sick and the drugs make
them feel better, but you can’t use them too often
because they cause worsening of the disorder over
time.”
This conundrum, Dr. Synowiec added, amounted
to a “huge issue” within the field of management of
headaches. “It’s been such an annoying thing for
everyone involved in migraine treatment to have to say,
‘Here are some pills that work, but you can only use
them so often,’” she said.
Under the leadership of director Dolores Santamaria,
MD, the Headache Center at the AHN Neuroscience
Institute has incorporated the latest, and perhaps most
promising, pharmacotherapies into clinical practice.
These treatments include novel agents called calcitonin
gene—related peptide receptor antagonists, or gepants,
which target pain-signaling molecules in the brain.
To date, two gepants have been approved by the FDA
for use as prophylaxis and/or treatment for acute
migraine, and Dr. Synowiec and her colleagues in the
Neuroscience Institute are using both agents, with
success (Headache 2020;60[5]:1037-1039).
The Headache Center treats patients with primary
headache disorder such as migraine, tension
headaches and cluster headaches as well as headaches
secondary to other medical conditions, including
allergies, traumatic brain injuries and sinus infections.
“These medicines are disease-modifying, meaning that
they should prevent acute migraine for those taking
them but also address the underlying mechanisms
causing the migraine,” Dr. Santamaria said.
In addition to encouraging patients to try these
emerging therapies, the AHN neurologists have been
using an internal registry of headache patients via data
built into electronic health records to monitor symptoms
and treatment side effects, such as fatigue, over time.
“This data allows us to look at disease markers such
as fatigue, sleep quality—things we don’t always have
time to ask about during examinations and can be
challenging to quantify,” Dr. Synowiec said. “We are
beginning to use this information to look at our patient
population and start to ask questions about whether
treatments not only improve symptoms but allow
patients to live their lives with migraine.”
 Throughout their nearly 30-year history, the residency
and fellowship programs offered through the Allegheny
Health Network’s (AHN’s) Neuroscience Institute have
emphasized traditional bedside teaching in all aspects
of the field, from basic neuroscience research to
neurosurgery.
Throughout their nearly 30-year history, the residency
and fellowship programs offered through the Allegheny
Health Network’s (AHN’s) Neuroscience Institute have
emphasized traditional bedside teaching in all aspects
of the field, from basic neuroscience research to
neurosurgery.
Specifically, the neurosurgery residency program
provides a broad-based education across all
neurosurgery subspecialties, and it is delivered via
clinical and didactic instruction as well as direct
surgical training. In addition, residents in the program
are actively involved in research and clinical trials
conducted through the Neuroscience Institute
and are given leadership training, all with an eye
toward preparing them to better serve their patients,
communities and leaders in medicine.
“The obvious goal of the program is [to] develop
residents into competent surgeons, but we also work with
them on their professional and personal development,
and position them to be future leaders of the field.” said
Jody Leonardo, MD, the director of the AHN Neurosurgery
Residency Program and director of the AHN Adult
Hydrocephalus Center. “The training is really in keeping
with our patient-centric approach to care.”
Through the seven-year program, which enrolls
two residents annually from a pool of more than
300 applicants from across the country and
around the world, residents are directly engaged
in patient care—initially under the guidance of
more experienced mentors and faculty—and
exposed to all of the neurosurgical specialties
offered at the AHN Neuroscience Institute, including
endovascular neurosurgery, stereotactic radiosurgery,
cerebrovascular neurosurgery, complex spine surgery
and skull base surgery.
 Neurosurgery residents at AHN are exposed to a wide
variety of learning opportunities during their residencies
that include clinical and didactic instruction as well
as surgical exposure and training. A core group of
faculty, all of whom are fellowship trained in specialty
ares, instruct and guide residents as they develop
and strengthen their clinical acumen while building
and enhancing surgical techniques. By the end of the
program, residents will have established a strong and
solid foundation of neurosurgery through which they
will be readily prepared to practice neurosurgery,
according to Dr. Leonardo.
Neurosurgery residents at AHN are exposed to a wide
variety of learning opportunities during their residencies
that include clinical and didactic instruction as well
as surgical exposure and training. A core group of
faculty, all of whom are fellowship trained in specialty
ares, instruct and guide residents as they develop
and strengthen their clinical acumen while building
and enhancing surgical techniques. By the end of the
program, residents will have established a strong and
solid foundation of neurosurgery through which they
will be readily prepared to practice neurosurgery,
according to Dr. Leonardo.
The curriculum focuses on practical physician
development topics including professionalism,
ethics, diversity and socioeconomics. Residents gain
practical experience in subspecialties such as plastic
surgery, trauma ICU, emergency department, neurocritical
care, pediatric neurosurgery, endovascular
neurosurgery, neuroradiology, stereotactic radiosurgery,
neuropathology and research.
“What we are striving to do through our residency
program is push the specialty of neurosurgery forward,”
said Alexander Yu, MD, the associate director of the
AHN Neurosurgery Residency Program and vice chair
of neurosurgery within the network. “You achieve that
by training residents with a focus on increasing our
knowledge base and improving patient care.”
“The obvious goal of the program is [to] develop residents into competent surgeons, but we also work with them on their professional and personal development, and position them to be future leaders of the field.”
——Jody Leonardo, MD, director, AHN Neurosurgery Residency Program
Copyright © 2023 All rights reserved. McMahon Group unless otherwise noted.
Reproduction in whole or in part without permission is prohibited.
McMahon Custom Healthcare Communications is part of McMahon Group.