 Welcome to the 2022 Allegheny Health Network (AHN)
Cardiovascular Institute annual report. We are excited
to share the highlights of our team and programs from
2022. We are very proud of the care and caring provided
to our patients and happy to share these highlights
and objective evidence of excellence.
Welcome to the 2022 Allegheny Health Network (AHN)
Cardiovascular Institute annual report. We are excited
to share the highlights of our team and programs from
2022. We are very proud of the care and caring provided
to our patients and happy to share these highlights
and objective evidence of excellence.
Readers of this issue will learn, for example, about AHN’s
Heart Failure program, whose quality is recognized by
the American Heart Association as among our nation’s
best, and will discover that the Joint Commission has designated
Allegheny General Hospital as a comprehensive
cardiac care center—its highest level of care and a recognition
attained by fewer than 20 programs nationwide.
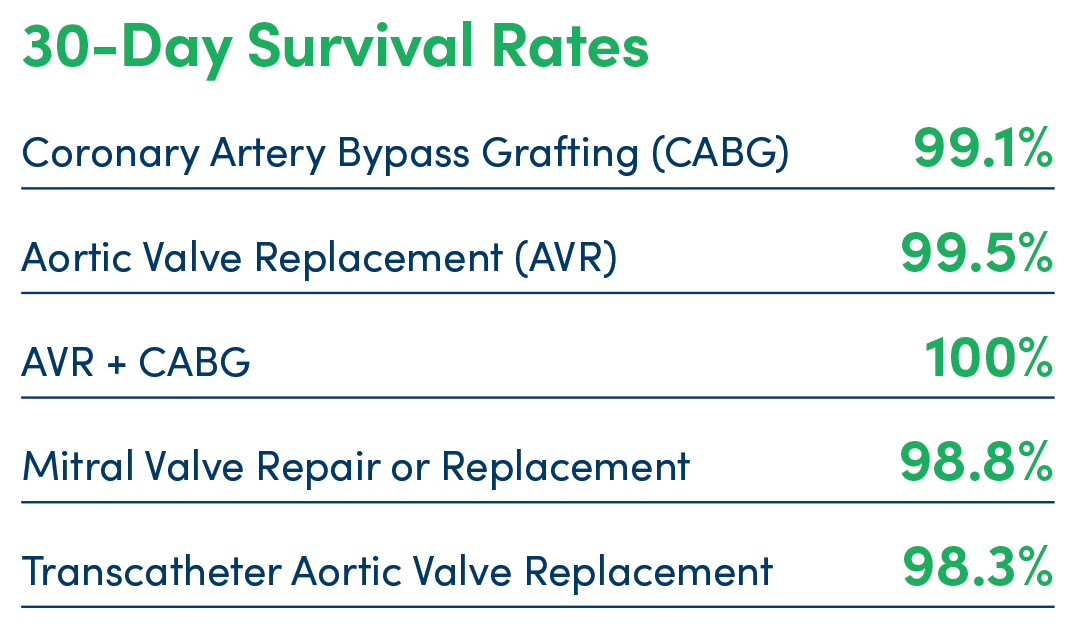
Meanwhile, the Society of Thoracic Surgeons (STS)
gave its highest rating of three stars to AHN’s Allegheny
General for four different cardiac surgical procedures:
coronary artery bypass grafting, transcatheter aortic
valve replacement, mitral valve repair/replacement
and aortic valve/coronary artery bypass graft surgery.
Allegheny General was recognized with a Mitral Valve
Repair Reference Center Award by the American Heart
Association® and The Mitral Foundation—one of just 22
in the country. The combined Allegheny General/Forbes
lung cancer program was also recognized by the STS as
a three-star program.
The AHN Cardiovascular Institute also has a robust
clinical research program dedicated to developing new and better ways to treat difficult
problems. This
allows patients to have early access to promising new
technologies and treatments. Physicians from around
the country routinely travel to AHN to learn these new
techniques from our teams.
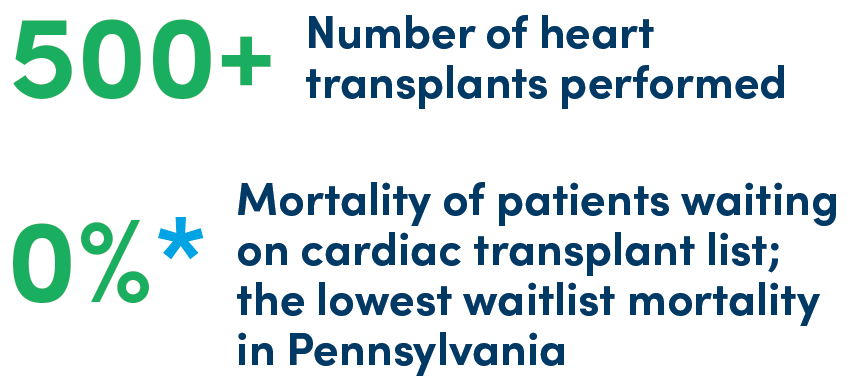
AHN’s expertise is demonstrated by the fact that the
Institute’s physicians and surgeons have amassed
impressive numbers for advanced procedures. AHN’s
transplant team recently performed their 500th heart
transplant.
We are grateful that these acknowledgments, and
others, confirm what we knew all along: that the
excellence of our physicians and surgeons and our
multifaceted, multidisciplinary care lead to great results
for our patients. Our culture of collaboration and
caring will continue to advance cardiovascular healthcare
at AHN.
You are invited to refer patients to our cardiovascular
programs or contact us for a consultation. Either way,
you will become part of a team working to optimize
your patient’s health.
Sincerely,
Stephen H. Bailey, MD
Chair, AHN Cardiovascular Institute
[email protected]
American Heart Association is trademarked and used with
permission.
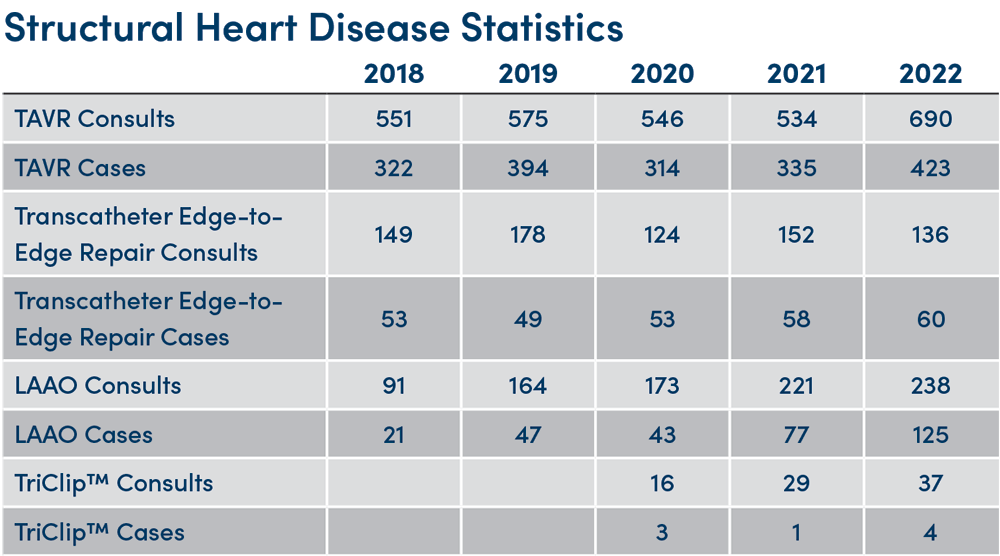
Approximately 2.5% of the U.S. population suffers from
valvular heart disease, a condition that causes about
25,000 deaths annually—most commonly from failure of
either the aortic or mitral valves.1
“If a patient is referred to Allegheny Health Network
[AHN] with valvular heart disease of any kind, we
will make sure that person gets to the right clinician
to diagnose, evaluate and treat the condition,”
said Stephen H. Bailey, MD, the chair of AHN’s
Cardiovascular Institute and the system chair of the AHN
Department of Thoracic and Cardiovascular Surgery.
“That’s done with a multidisciplinary, collaborative heart
team.”
AHN is highly experienced and nationally recognized for
treating valvular heart disease in all its forms. Allegheny
General Hospital—the flagship academic medical
center of AHN—was given the prestigious three-star
rating from the Society of Thoracic Surgeons (STS) for both its transcatheter aortic valve
replacement (TAVR)
program and its aortic valve/coronary artery bypass
graft surgery program. AHN has also been recognized
as one of only twenty-two centers in the country to
receive the Mitral Valve Repair Reference Center Award
for excellence by the American Heart Association® (AHA)
and the Mitral Foundation, and is also designated a
three-star program by the STS.
Among other areas, Dr. Bailey specializes in aortic
stenosis. “We tailor the procedure to the patient’s
specific aortic valve problem,” he said. “That includes
traditional open-heart surgery, minimally invasive
surgery or transcutaneous valvular interventions.” The
exact procedure is dictated by the patients’ specific
medical circumstances and anatomy.”
 Surgical aortic valve replacement (SAVR), which can be
performed as either an open-heart or minimally invasive
procedure, until recently was the treatment of choice for severe aortic stenosis. Most
patients are able to go
home in 4 days. Although SAVR has been the standard
approach for replacing a diseased heart valve, research
performed at AHN has helped demonstrate the efficacy
of non-invasive procedures like TAVR. TAVR is performed
by a team of specialists without the need for incisions or
general anesthesia, and patients usually go home the
day after the procedure.
Surgical aortic valve replacement (SAVR), which can be
performed as either an open-heart or minimally invasive
procedure, until recently was the treatment of choice for severe aortic stenosis. Most
patients are able to go
home in 4 days. Although SAVR has been the standard
approach for replacing a diseased heart valve, research
performed at AHN has helped demonstrate the efficacy
of non-invasive procedures like TAVR. TAVR is performed
by a team of specialists without the need for incisions or
general anesthesia, and patients usually go home the
day after the procedure.
“ With the robotic approach—where
we’re operating between the ribs and
no broken bones are involved—most
people are back to work within a
month.”
—Walter E. McGregor, MD, AHN’s Director,
Cardiac Surgery Division
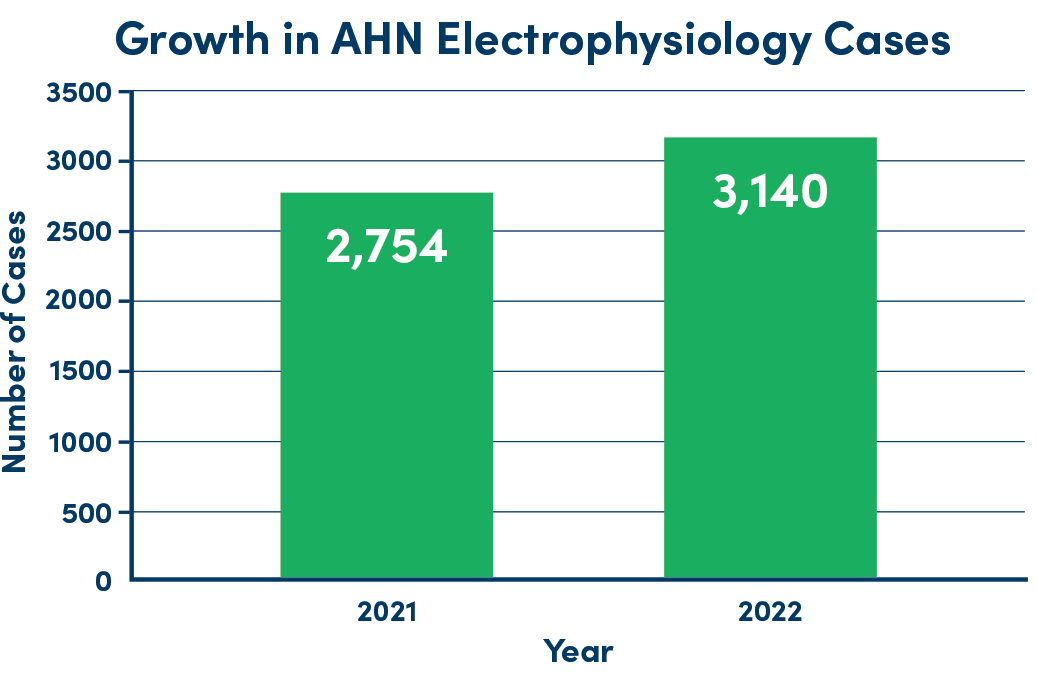
 The electrophysiology experts at Allegheny Health
Network (AHN) take a comprehensive approach for
treating even the most difficult heart rhythm problems.
The electrophysiology experts at Allegheny Health
Network (AHN) take a comprehensive approach for
treating even the most difficult heart rhythm problems.
“Our electrophysiology program has a very sharp focus
on efficacy and safety,” said Amit J. Thosani, MD, the
director of cardiac electrophysiology for AHN and vice
chair of the AHN Cardiovascular Institute.
To help achieve these goals, Dr. Thosani and
his colleagues incorporate state-of-the-art
electrophysiologic technology into the diagnosis and care
of their patients. This includes a low- or no-fluoroscopy
approach to catheter ablation, which minimizes patient
exposure to radiation during these procedures.
The electrophysiology experts also integrate advanced
mapping and imaging systems into their practice,
an innovation that virtually eliminates the need for
preprocedural imaging, thereby reducing the number
of visits that patients need to make to the hospital.
High-power, short-duration catheter ablation leads to
improved lesion creation, with less risk for damage to
surrounding structures. Leadless pacemakers are also
among some of the newer devices used in AHN’s cardiac
electrophysiology practice, as well as conduction system
pacing that uses the heart’s natural electrical pathways
to create more physiologic pacing conditions.
“We are fortunate to host physicians from around the
country who come to observe how we operate,” Dr. Thosani
pointed out. “So, we lead, we innovate and we teach.”
AHN offers a comprehensive continuum of care for
patients with arrhythmias, which begins the moment
a patient first develops symptoms, and continues
through diagnosis, medical/surgical management and
postoperative care. At AHN, treatment includes not only
that for refractory arrhythmias that have not responded
to traditional therapies, but also advanced surgeries,
which are performed in conjunction with the network’s
cardiovascular surgeons.
Ultimately, it’s the combination of all these features that
makes AHN’s electrophysiology department a smart
destination for patients throughout the region. “We offer
the full gamut of arrhythmia care,” Dr. Thosani noted. “As
a complete cardiac care referral center, we treat patients
both with de novo arrhythmias as well as those who have
had treatments elsewhere and are still having rhythm
issues,” Dr. Thosani said. “There are very few things we
cannot treat.”
Allegheny Health Network (AHN) has one of the premier
programs for heart failure (HF) in the United States, and
is experienced in virtually every aspect of HF diagnosis
and treatment—excellence that has been recognized by
the American Heart Association®.
As part of its 360-Degrees of Care Program, AHN’s
Heart Failure Clinic offers patients access to a wide
range of cutting-edge medical, surgical and device
treatment options, as well as mechanical circulatory
support and cardiac transplantation.
“Ours is a very large and diverse program,” said
Manreet Kanwar, MD, the director of AHN’s Mechanical
Circulatory Support and Transplant Program. “It is a
patient-centered program that practices an evidencebased
approach, with multiple professionals working
together on behalf of the patient.”
This approach enables Dr. Kanwar and her colleagues
to target subgroups of patients who require special
attention, particularly those with uncommon causes
of cardiomyopathy, such as amyloidosis, hypertrophic
cardiomyopathy, inherited cardiomyopathy, etc.
Hypertrophic cardiomyopathy can sometimes result in
life-threatening arrhythmias or sudden death, yet many
patients present with few, if any, symptoms and the
condition is difficult to diagnose. In recent years, AHN’s
hypertrophic cardiomyopathy program, led by Craig
Alpert, MD, and Pietro Bajona, MD, PhD, has grown
rapidly, becoming an important regional referral center
with a burgeoning national reputation.
Dr. Kanwar’s team continues to develop expertise and
enhance its reputation in the field of advanced heart
failure and cardiogenic shock. For decades, cardiogenic
shock has had a fatality rate of approximately 50%.1,2
Given this risk, treatment requires a focused, organized
multispecialty approach to address the needs of these
patients in critical moments.
AHN has organized a “hub and spoke” model to help
triage and transfer patients in any regional center who
present in cardiogenic shock. “With this program, our
shock survival rate over the past year was over 60%, which
is far better than traditional statistics,” Dr. Kanwar said.
Another innovative program, led by Matthew Lander,
MD, and Azam Hadi, MD, treats patients with cardiac sarcoidosis, an uncommon yet potentially
deadly
inflammatory condition in which granulomas form in
heart tissue, interfering with normal heart function and
potentially causing arrhythmias, cardiomyopathy or
heart failure.
Dr. Kanwar and her team are known for their expertise
in “advanced” heart failure, but also are committed to
prevention and early detection of disease—an approach
that often takes advantage of rapidly evolving remote
monitoring, including implantable and wearable
devices.
Implantable technology aims to leverage and
integrate data from such devices as defibrillators and
pacemakers. An example of this technology is the
CardioMEMS™ implantable hemodynamic monitor,
which provides early warning of HF decompensation
and may help to prevent hospitalization.
Advances in wearable technology—from external
patches to devices like the Fitbit® and Apple Watch®—
also allow AHN physicians to remotely assess patient
wellness.
“Leveraging this technology ensures that we can
recognize problems as soon as they occur, and develop
solutions before these patients end up in an emergency
room or require hospitalization,” Dr. Kanwar said.
Despite treatment, HF progresses to an advanced stage
in some patients. For these individuals, AHN offers
therapeutic options such as mechanical circulatory
support and cardiac transplantation—procedures
that demand the highest level of clinical expertise.
Mechanical circulatory support supplements or
replaces the action of the failing heart using a variety
of technologies, including temporary options such as
extracorporeal membrane oxygenation, intra-aortic
balloon pumps, and the Impella® or TandemHeart®
devices, or long-term therapies such as left ventricular
assist devices (LVADs).
“These surgeries, both of which we offer here,
require a high level of expertise and ICU care in a
multidisciplinary fashion,” said Masaki Tsukashita, MD,
PhD, the surgical director of the Mechanical Circulatory
Support and Cardiac Transplantation programs at AHN.
 In a small subset of patients with advanced HF, the only viable therapeutic option is
cardiac transplantation.
While the procedure is exceptionally complex,
Drs. Kanwar and Tsukashita and their teams are
approaching an important milestone: They will soon
perform their 500th heart transplant. This extensive
experience is one reason why AHN is designated by The
Joint Commission® as a comprehensive cardiac care
center—the highest possible level of care.
In a small subset of patients with advanced HF, the only viable therapeutic option is
cardiac transplantation.
While the procedure is exceptionally complex,
Drs. Kanwar and Tsukashita and their teams are
approaching an important milestone: They will soon
perform their 500th heart transplant. This extensive
experience is one reason why AHN is designated by The
Joint Commission® as a comprehensive cardiac care
center—the highest possible level of care.
“Not many health systems are certified for both
mechanical circulatory support and cardiac
transplantation as a treatment option for advanced
cardiac disease,” Dr. Kanwar said.
As a complex, multifaceted condition and a chronic
disease, HF requires a lifelong approach to care. “No
matter where the patients are on their journey, we have
developed the processes and programs that allow them to get the finest long-term care
possible and achieve
the best possible outcomes,” Dr. Kanwar said.
1.J Am Heart Assoc
2021;10(15):e021061.
2. tctmd.com/news/hospital-mortality-hasnt-budged-despitechanges-
mcs-cardiogenic-shock.
American Heart Association is trademarked and used with
permission.
CardioMEMS is a trademark of Abbott Laboratories and is used with
permission.
Fitbit is a trademark of Google and is used with permission.
Apple Watch is a trademark of Apple and is used with permission.
Impella is a trademark of OSF HealthCare and is used with
permission.
TandemHeart is a trademark of LivaNova and is used with
permission.
The Joint Commission is trademarked and used with permission.
Allegheny Health Network Cardiovascular Institute physicians are involved in multiple
clinical trials.
Here is a sampling of a few, and why the study is noteworthy:
 *
www.srtr.org/transplant-centers/allegheny-general-hospital-paa
g/?organ=heart&recipientType=adult&donorType=
*
www.srtr.org/transplant-centers/allegheny-general-hospital-paa
g/?organ=heart&recipientType=adult&donorType=
 Source: Society of Thoracic Surgeons 2021 report
Source: Society of Thoracic Surgeons 2021 report
 Coronary artery disease treatment at Allegheny Health
Network (AHN) starts with medical management, the
particular expertise of Indu Poornima, MD, the director
of nuclear cardiology at AHN.
Coronary artery disease treatment at Allegheny Health
Network (AHN) starts with medical management, the
particular expertise of Indu Poornima, MD, the director
of nuclear cardiology at AHN.
“The philosophy behind the medical management of
coronary disease at AHN is that by adequately treating
the underlying disease process, we can prevent or
hinder its progression,” Dr. Poornima said. This involves
the mitigation of risk factors such as high cholesterol,
high blood pressure, diabetes, smoking, obesity and
stress, she added.
The evidence in favor of medical management of
coronary artery disease is compelling, Dr. Poornima
said, and founded on two landmark investigations, the
COURAGE trial1 and the ISCHEMIA
trial,2 which together
demonstrated that medical management of coronary
artery disease is at least comparable to more invasive
therapeutic approaches in certain patient populations.
“I think there’s been a paradigm shift in the way we
approach this disease,” Dr. Poornima explained, “and
it really speaks to the whole concept of preventive
cardiology, which plays a huge role in the management
of coronary disease.”
David M. Lasorda, DO, the director of interventional
cardiology at AHN, and his colleagues use catheterbased
approaches to treat coronary artery disease and
structural heart disease.
The interventional cardiologists are skilled at diagnostic
angiograms and interventional procedures such as
angioplasty, with stenting usually performed through
the radial artery at the wrist.
“We perform the entire range of diagnostic and
therapeutic procedures, from very straightforward to
extremely complicated. However, the hallmark of our
program is the really challenging patients that have
been turned down elsewhere and then referred to AGH
for another opinion.
“We’ve worked hard to ensure that we can treat virtually
any patient that walks or wheels in our doors,” Dr.
Lasorda said.
Of course, there are instances where the severity
of a patient’s disease requires more than nonsurgical
management. When surgery is a patient’s
best option, they can turn to AHN’s cardiothoracic surgeons, including M. Scott Halbreiner,
MD, whose
expertise spans virtually every procedure available.
Dr. Halbreiner can perform coronary artery bypass
graft (CABG) surgery for patients with coronary artery
disease as either a traditional open or minimally
invasive procedure.
Most of AHN’s coronary artery disease interventions are
multidisciplinary efforts, which Dr. Halbreiner sees as
a tremendous advantage for his patients, particularly in the complex cases in which he and
his colleagues
specialize. Patients can be confident that they are
getting the expert opinion of an entire team and a
solution carefully crafted to their specific situation.
“We can have as many as 12 professionals discussing a
patient to help formulate a strategy and a care plan,”
Dr. Halbreiner said. Such efforts, he added, also include
the critical, postoperative period.
AHN’s expertise has been recognized by its 3-star
rating for CABG surgery from the Society of Thoracic
Surgeons, an achievement reserved for only the finest
programs in the country and which few other institutions
can claim.
“It means our CABG surgery program is in the top tier in
the country in terms of outcomes,” Dr. Halbreiner said.
“What’s more, it’s a rating we’ve maintained for several
years now.”
Whether it’s recognition by the most prestigious
professional body in the country, a multidisciplinary
approach to disease prevention or innovative
therapeutic techniques, coronary artery disease
treatment at AHN is a multifaceted affair, where all
patients will find a dedicated team prepared to work
hard to ameliorate their disease process.
1. N Engl J Med 2007;356[15]:1503-1516.
2. N Engl J Med 2020;382[15]:1395-1407.

 The vascular surgeons at Allegheny Health Network
(AHN) employ the latest innovations, including
transcervical carotid stenting, a minimally invasive
surgical technique that is quickly becoming the gold
standard for treatment of carotid artery disease.
The vascular surgeons at Allegheny Health Network
(AHN) employ the latest innovations, including
transcervical carotid stenting, a minimally invasive
surgical technique that is quickly becoming the gold
standard for treatment of carotid artery disease.
Also known as transcarotid artery revascularization
(TCAR), the procedure is performed via a tiny incision in
the neck, through which the surgeon works to stabilize
plaque from inside the artery and restore normal blood
flow to the brain.
“Carotid endarterectomy has historically been the gold
standard for treating carotid stenosis,” explained Satish
C. Muluk, MD, the director of the Division of Vascular
Surgery at AHN. “Although it has very low rates of
serious complications like stroke and death, it has to be
performed under general anesthesia.” TCAR also avoids
the potential for cranial nerve injury.
The incidence of major adverse events such as stroke
and death is even lower with TCAR than carotid
endarterectomy.1
Recently, Dr. Muluk and his colleagues performed their
300th TCAR procedure, making AHN one of the most
active TCAR centers in the country. The department
has tracked patient outcomes through the Society for
Vascular Surgery® Vascular Quality Initiative® clinical
registry and found incidence rates of death or stroke to
be less than 1%.2
The vascular surgery team at AHN has abundant
expertise in repairing abdominal aortic aneurysms
(AAA), using both open and endovascular surgery. An
open repair replaces the aneurysm with a synthetic graft. Endovascular aneurysm repair uses
a catheter to
place a stent and graft to support the aneurysm.
“Endovascular aneurysm repair is not appropriate for
everyone,” Dr. Muluk said. “There are patients whose
aneurysms just aren’t well suited for an endovascular
approach, and we can’t sacrifice outcomes just for
convenience.”
For this reason AHN strikes a balance between both
approaches to AAA repair—a philosophy that allows
surgeons to maintain their skills in each.
“You should not be a hammer looking for a nail, and
you shouldn’t always be looking for an endovascular
solution,” Dr. Muluk said. “Because if you do that, then
you risk losing your familiarity and comfort with open
surgery.”
An exciting innovation in endovascular AAA repair is
IOPS®, for Intra-Operative Positioning System. This
technology offers several advantages, including less
patient exposure to radiation and contrast dye.3
“The beauty of the IOPS system is that it allows us
to perform anatomically complex catheterization
procedures without fluoroscopy,” Dr. Muluk noted. “We’re
currently in the process of analyzing when and how we
use it so that we maximize the benefits of the technology.”

There is no more prestigious recognition for a thoracic
surgery program than receiving a three-star rating from
the Society of Thoracic Surgeons, which is precisely
the distinction earned by Allegheny Health Network’s
(AHN’s) Allegheny General and Forbes hospitals for lung
cancer resection.
“There are only 27 three-star programs in the nation,”
said Benny Weksler, MD, the system chief of thoracic
surgery at AHN. “And here in western Pennsylvania,
there is no other.”
AHN’s clinical expertise is not limited to the operating
room. One of the hallmarks of AHN’s lung cancer
initiative is its comprehensive screening program, a vital
component for a disease that is typically not discovered
until it has reached incurable stages. AHN’s robust
screening initiatives lead to early detection, which can
significantly reduce mortality.
Another important factor is that each patient’s care is
truly multidisciplinary, which allows AHN’s surgeons,
interventional pulmonologists, medical oncologists and
radiologists to decide together the best course of action.
Often, this does not lead to surgery.
“If the findings of those screenings are not discussed
at length, then you may end up having many more
patients undergoing surgery than is necessary,” Dr.
Weksler said. Nonsurgical treatment regimens include
chemotherapy, immunotherapy and radiation therapy.
Thoracic conditions treated at AHN include lung cancer
as well as esophageal cancer and benign esophageal
disease. If surgery is required for malignant disease,
physicians such as Hiran Fernando, MD, the director of
thoracic surgery at Wexford Hospital, are experts in the
use of minimally invasive techniques, such as videoassisted
thoracoscopic surgery.
“Minimally invasive approaches to esophageal cancer
have a lower risk for pneumonia and infections, and
quicker return to normal activity,” Dr. Fernando said.
There have also been significant advances in minimally
invasive therapies for benign disease. For instance,
the implementation of the cutting-edge LINX® reflux
management system for a weak gastroesophageal
sphincter and hiatal hernia. Similarly, transoral
incisionless fundoplication is an endoscopic procedure
used to treat disorders such as gastroesophageal reflux
disease, and peroral endoscopic myotomy is effective
for patients with muscle disorders of the esophagus,
such as achalasia.
This variety of surgical and nonsurgical approaches
helps AHN’s thoracic surgeons tailor their therapeutic
approach for any patient. AHN also has a robust clinical
trials program offering patients early access to the most
important and effective new therapies.
 In 2015, Allegheny Health Network (AHN) became the
first center in western Pennsylvania to be certified as a
Pulmonary Hypertension Care Center by the Pulmonary
Hypertension Association—a designation it carries
today.
In 2015, Allegheny Health Network (AHN) became the
first center in western Pennsylvania to be certified as a
Pulmonary Hypertension Care Center by the Pulmonary
Hypertension Association—a designation it carries
today.
“We care for all forms of pulmonary hypertension,”
said Amresh Raina, MD, the associate medical
director of AHN’s Pulmonary Hypertension Program,
including pulmonary arterial hypertension, pulmonary
hypertension related to left-sided heart disease,
pulmonary hypertension related to interstitial lung
disease and hypoxia and chronic thromboembolic
pulmonary hypertension (CTEPH).
One exciting development in the management of
pulmonary hypertension due to interstitial lung disease
is treprostinil, a synthetic analog of prostacyclin. AHN
participated in INCREASE,1 a
landmark study that found
treatment with the novel agent improved participants’
physical exercise capacity.
“This was a significant development,” Dr. Raina
explained. “Previously, there was no treatment for
these patients, and they were instead referred for lung
transplantation, assuming they were viable candidates.”
Gone are the 1990s, when there was one FDA-approved
medication—a continuous prostacyclin infusion. “Now
there are 14 FDA-approved drugs, which we usually use
in combinations to maximize their effectiveness and
utilize potential synergistic effects,” Dr. Raina said.
Of the different forms of pulmonary hypertension
treated at AHN, one of the rarest is CTEPH. AHN is
one of only a handful of elite medical programs in the
country—and the only one in western Pennsylvania—
with the expertise to perform two highly advanced
surgical procedures to treat CTEPH.
The procedures are percutaneous balloon pulmonary
angioplasty and surgical pulmonary endarterectomy,
the latter of which is curative for CTEPH. For eligible
candidates, pulmonary endarterectomy is the gold
standard treatment for the surgical removal of blood
clots and scar tissue in the pulmonary arteries.
“CTEPH has a nuanced disease process and is often
underdiagnosed,” said Candice Lee, MD, a cardiac
surgeon at AHN, who specializes in pulmonary
thromboendarterectomy. As Dr. Lee explained, the
smaller, more distal clots that often characterize CTEPH are especially difficult to remove
and require
exceptional technique and judgement.
Dr. Lee and her colleagues are rapidly approaching
their 100th pulmonary thromboendarterectomy, with a
survival rate of 100% at the time of this writing.

Copyright © 2023 All rights reserved. McMahon Group unless otherwise noted.
Reproduction in whole or in part without permission is prohibited.
McMahon Custom Healthcare Communications is part of McMahon Group.